By Michelle Wright, CEO & founder of mishfit
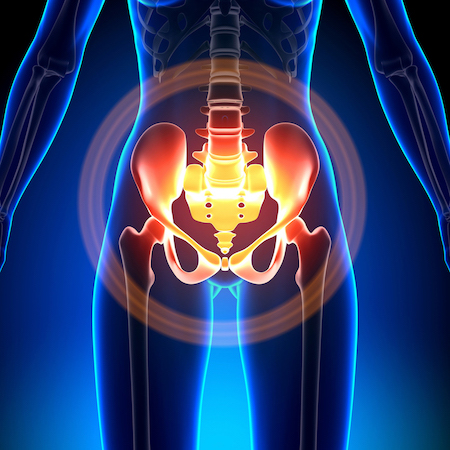
Pelvic floor dysfunction can vary greatly from woman to woman, with sometimes the symptoms being surprising similar.
It is absolutely essential that women are given the correct diagnosis of their pelvic floor dysfunction by a professional – such as a Women’s Health Physiotherapist or gynecologist, before they undertake an exercise option.
Here are some of the most common pelvic floor dysfunction issues:
- Urge incontinence:
When you need to go, you need to go! Women who experience urge incontinence often “go to the toilet, just in case” (Hint! A big no no!) or are familiar with all the toilets in their usual routes outside the house. If unaddressed women can often “opt” out of things, simply because the anxiety of not knowing where a toilet is.
On a physical level your pelvic floor needs to train the long twitch muscle fibres (like an endurance runner). A great tip when suffering urge incontinence – give you pelvic floor a series of quick contractions. This can trick your brain and give you a good 5 to 10 minutes to calmly find a toilet.
My advice is also is to notice your self-talk – if you internal dialogue is “I’m going to wet my pants! I’m going to wet my pants” – chances are you will!
- Stress incontinence:
Leaking a little wee when you laugh, cough, move quickly, including, changing direction. This requires training the short twitch, or sprint function of your pelvic floor. Learning to contract quickly and practice your timing is important. To retrain the body, break down the functions and re-coordinate the body, consciously at first. For example, contract pelvic floor, force a cough and then release pelvic floor. With time and practice, your body will learn better timing and will catch before it needs it, rather than after as an unconscious function.
- Prolapse:
Prolapse means “fall out” and happens when the uterus, bladder or bowel falls out of place and into and sometimes through the vaginal opening. Statistics from Continence Foundation of Australia report prolapse affects around 50% of postnatal women. There are many factors that influence prolapse – hormonal changes (like that of child bearing and menopause), hereditary factors (prolapse runs in families), a history of heavy lifting, childbirth, lax ligament makeup and high impact exercise.
Prolapse may be a physical condition. But prolapse also effects mental and emotional well-being. To deal with prolapse effectively, it needs to be dealt with holistically. This includes addressing toileting behaviour and how women go about their functional day and how they exercise. Addressing incontinence and prescribing pelvic floor safe exercises is essential.
- Hypertonic pelvic floor:
Hypertonic pelvic floor is when the pelvic floor does not switch off. For a pelvic floor muscle to be effective it needs to turn on and turn off when needed. Having a hypertonic pelvic floor that does not switch off may lead to incontinence, painful sex and re-occurring urine infections.
For women who have a hypertonic pelvic floor they need to learn to down train their pelvic floor. This includes relaxation techniques and making sure that they are not bracing their pelvic floor continually during exercise and their day.
- Vulvadynia:
Can be described as the pain, often unexplained in the vulva (around the entrance to the vagina). There is often no singular cause and often sufferers also are diagnosed with depression. Which is not surprising, as I would feel pretty depressed if my vulva felt pain constantly.
Vulvadynia can be explained as the body confusing signals with pain in the mind. Vulvadynia can also be responsible for painful sex.
- Vaginismus:
This can often be confused with vulvadynia, but this is more a muscle spasm on anything penetrating the vagina (penis, tampons or when undergoing a pap smear). For some women even the mere thought of penetration can bring on the painful muscular spasms. It is involuntary and the severity can vary greatly from woman to woman. Unfortunately the pain from sexual penetration is likely to remain until the vaginismus is addressed.
There can be many reasons for both Vaginismus and vulvadynia – sexual assault, ongoing yeast infections, stress, anxiety, and may need “down training” (i.e.: similar to a hypertonic pelvic floor). It helps to go to a Women’s Health physiotherapist who is experienced in pelvic pain and with these sort of issues.
- Any pelvic floor pain:
For whatever reason, if there is any ongoing pelvic pain – I recommend you address it. Just like ignoring incontinence can possibly leading to prolapse – pelvic pain can possibly lead to vulvadynia and / or vaginismus.
Remember prevention is much easier than cure.
You might also like to read:
Top 10 tips for creating a body positive culture for you and your children
How to do pelvic floor exercises